A hospital system is a complex ecosystem, comprised of many distinct roles working in coordination to deliver care.
On any given day, that ecosystem may include nurse practitioners supporting clinical decision-making, schedulers coordinating appointments, call center staff handling urgent patient questions, and revenue cycle teams navigating coverage requirements. Think about it this way: the average patient and their family may interact with 15-20 members of the hospital team on average – even for an outpatient procedure.
Hospitals are also the cornerstone of a broader healthcare ecosystem that employs over 17 million people in the United States – the largest employment segment in America.
Still, human capital and workforce challenges abound in the hospital ecosystem: close to 50% of clinicians routinely experience burnout, with an annual average turnover rate close to 30% for some hospital roles.
These conditions warrant a comprehensive set of solutions – and one of them is better training.
The current state of workforce training in hospital systems
Within a hospital system, multiple layers of training operate in parallel.One layer consists of the mandatory education and credentialing required for physicians, nurses, and other licensed clinicians. This can include anything from formal postgraduate training programs to hands-on clinical training, and are essential to safe clinical practice.
Alongside this, hospital systems also rely on a separate layer of system-level workforce training that supports day-to-day operations across both clinical and non-clinical roles. This training can include:
- Onboarding programs that orient new employees to the organization, including core policies, system access, and expectations for how work gets done
- Compliance and regulatory training required to meet safety, privacy, and accreditation standards.
- Operational and role-readiness training that defines how specific roles are expected to handle recurring situations like patient communications, billing and scheduling inquiries, or documentation.
In most hospital systems, components of this system-level training are delivered through centralized learning infrastructure, such as a healthcare learning management system (LMS) or compliance platform, designed to scale across a diverse workforce. Additional training and onboarding may happen through synchronous, human-led training sessions that require dozens of hours of staff time.
For example, a new hire – regardless of whether they’re in a clinical or non-clinical role – might move through a standardized onboarding pathway through their LMS that combines mandatory modules (e.g., HIPAA training and safety protocols) with baseline instruction on organizational expectations and technology access.
While this centralized approach is common across hospital systems, the training often falls short.
The problem with traditional training in hospital systems
While designed to support training needs at scale, traditional training programs often introduce challenges to healthcare systems:
There’s a clear disconnect from real-world practice
Traditional training fails to capture the complexity of healthcare work. System-level training is frequently delivered through static content like slide decks, recorded modules, or policy documentation. These materials, while informational, don’t show how decisions unfold in context or enable immersive practice opportunities.
For operational and patient-facing roles, this gap is especially pronounced. Static training often introduces policies, procedures, and escalation guidelines related to billing, scheduling, and patient communication.
But applying that guidance – such as resolving a billing concern, coordinating schedule changes across departments, or escalating an urgent patient issue – requires judgment, timing, and cross-team coordination. When training stops at generalized instruction, employees are left to bridge that gap on the job, exposing them to costly (or at worst, lethal) mistakes down the line.
The limits to static training are well-documented: the CDC reports that up to 70% of content and knowledge is lost when training relies on more static models, proving the value and necessity of more immersive learning models.
Efficacy is challenging to measure
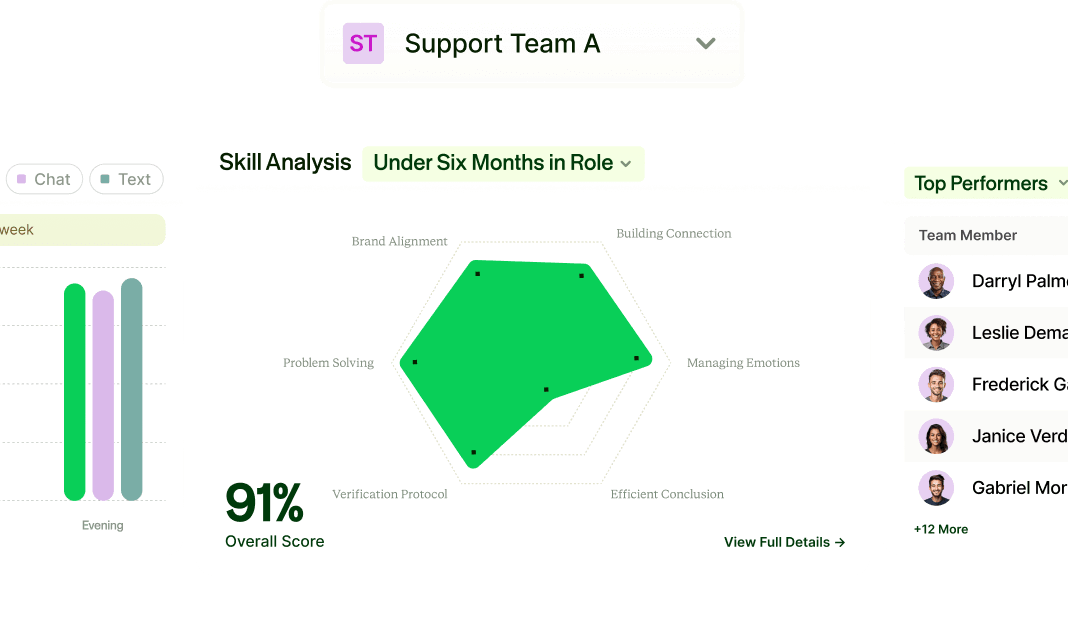
Another core failure of traditional training is how it measures trainee effectiveness. Many programs rely on LMS-driven metrics like course completion, attendance, or post-training satisfaction surveys.
While these measures are easy to track and report, they have little to no correlation to whether employees can actually apply policies, follow workflows, or navigate complex operational scenarios in their roles. This is a documented challenge across the space – almost 60% of healthcare professionals in one study lack clear ways to evaluate training efficacy.
Without performance-based measurement, hospital leaders will lack visibility into readiness gaps and allocate their resources in ineffective ways.
System-level training creates downstream costs
On paper, more static training programs seem cost-effective. However, as the two points above illustrate, many of those costs are often shifted downstream rather than eliminated.
When employees complete required training without being able to apply it effectively on the job, the impact extends beyond the individual learner. Errors are more likely, processes break down, and more experienced staff have to be pulled into reactive scenarios to answer questions or correct mistakes.
Over time, these gaps can contribute to operational friction and higher turnover as employees feel unprepared to meet day-to-day demands. This is especially dangerous from the standpoint of turnover cost – close to 40% of employees who leave in the first year do so (voluntarily or otherwise) because of lack of role readiness, in turn driving serious hiring and retraining costs incurred.
Soft skills are ignored – causing brand risk
While hospital training systems often focus on policies (such as those required to align with compliance standards), and hard skills (like EHR updates), they systematically ignore training on softer skills that are core to customer service in any healthcare function.
For any patient- or customer-facing role in hospitals – from doctors to billing associates – effective customer care is essential to overall performance. ReflexAI’s research indicates that agents who show strong interpersonal skills (such as empathy) early on are better performers across a wide range of skills throughout their tenure.
Still, centralized training systems typically overlook opportunities for staff to practice empathy, trust building, and other softer skills that are core to effective customer service.
This causes a real brand risk in healthcare settings: put simply, patients who get bad service in hospitals will choose other providers in the future. This isn’t limited to clinical care gaps: one study shows that more than half of patients will likely switch providers after a poor billing experience.
AI-powered simulations: A potential solution for workforce learning across hospital systems
Interactive, simulation-based, workplace learning has long been used in healthcare to support skill development and decision-making.
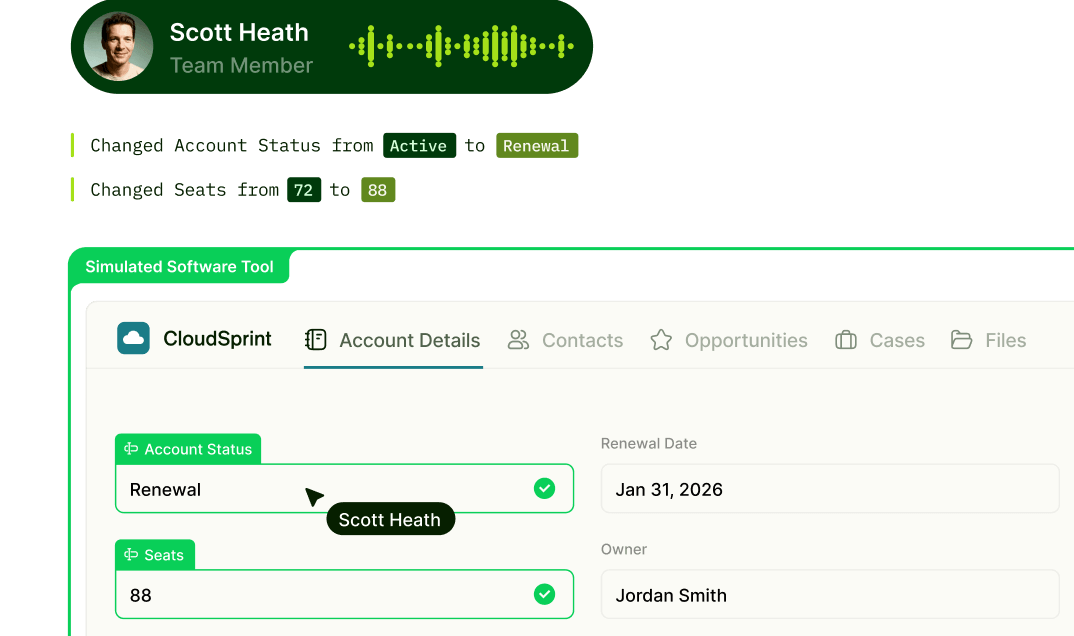
When applied to system-level workforce training, AI-powered simulations extend these benefits by allowing employees to practice how policies, workflows, and escalation protocols play out in realistic, role-specific scenarios.
Specifically, with AI-driven simulations, healthcare systems can:
- Recreate complex, role-specific scenarios that reflect real clinical, operational, or administrative challenges.
- Provide low-risk practice environments where learners can build fluency and judgment without impacting patient care.
- Adapt to individual learner needs and deliver personalized, engaging training experiences.
- Provide data and performance-based insights that allow for personalized coaching.
As health systems look to operationalize AI-based learning at scale, the question shifts from whether simulations work to how to evaluate and select the right technology to support them.
Critical things to consider when acquiring AI-powered simulation technology – a checklist
When vetting an AI-powered simulation platform, go beyond surface-level features. To know what to look for, we put together a short, practical checklist to guide the decision-making process:
Security needs
Hospital systems operate under strict regulatory frameworks, so any platform should be able to:
- Safeguard ePHI, patient scenarios, and training data with robust privacy and breach-notification controls.
- Demonstrate compliance with HIPAA’s privacy and security rules and attest to how data is stored, encrypted, and processed.
- Show independent security validation, such as SOC 2 or ISO 27001 certifications, and explain how third-party components handle data.
Clinical context
An effective AI simulation platform also has to capture the nuances of clinical, operational, and administrative work inside a healthcare system. Specifically, choose a tool that has:
- Operated in healthcare-specific or other high-stakes environments.
- Accurately reflects real-world workflows, language, and decision points (e.g. patient communication, documentation, etc.)
- Supports regulated scenarios where compliance, safety, and accuracy are critical.
Self-serve
In hospital systems, standardizing training across functions requires entirely different personas. That’s why it’s critical for a platform to have self-serve capabilities that allow the:
- Creation and adjustment of role-specific scenarios (e.g. nurse triage, scheduler workflows, etc.)
- Customization of scoring rubrics and feedback frameworks that align with organizational goals.
- Rapid iteration without heavy vendor dependency.
Examples of how AI-powered simulations can be used in a hospital setting
AI simulations can be used across a wide variety of roles and scenarios within the hospital system. Below are a few examples of specific use cases.
Role / Function | Example Simulation Use Cases | Skills Developed |
Clinical staff (within system-level training) | Patient communication, applying organizational policies during patient interactions, navigating EHR workflows, coordinating handoffs, escalating non-routine issues | Effective communication, policy application, workflow adherence, cross-team coordination, documentation accuracy, empathy and soft skills |
Nursing Staff (operational readiness) | Patient communication, shift handoffs, patient education conversations, responding to workflow exceptions, coordination with ancillary teams | Situational judgment, communication, process execution, escalation |
Administrative Staff | Scheduling conflicts, prior authorization workflows, coordination with clinical and revenue cycle teams | Process navigation, problem-solving, cross-functional communication |
Hospital Call Centers & Information Desks | Appointment changes, billing questions, privacy-sensitive conversations, escalation of urgent concerns | Information gathering, de-escalation, policy-compliant communication, decision escalation |
Revenue Cycle & Claims Management | Benefits explanations, documentation requirements, compliance-sensitive interactions with patients and payers | Regulatory awareness, accuracy, escalation judgment, policy adherence |
Use ReflexAI to power training across your hospital system
With AI-powered simulations, you can transform your training infrastructure to one that replicates real-world complexity, encourages a safe practicing environment, and gives managers access to the data they need to invest wisely in workforce development.
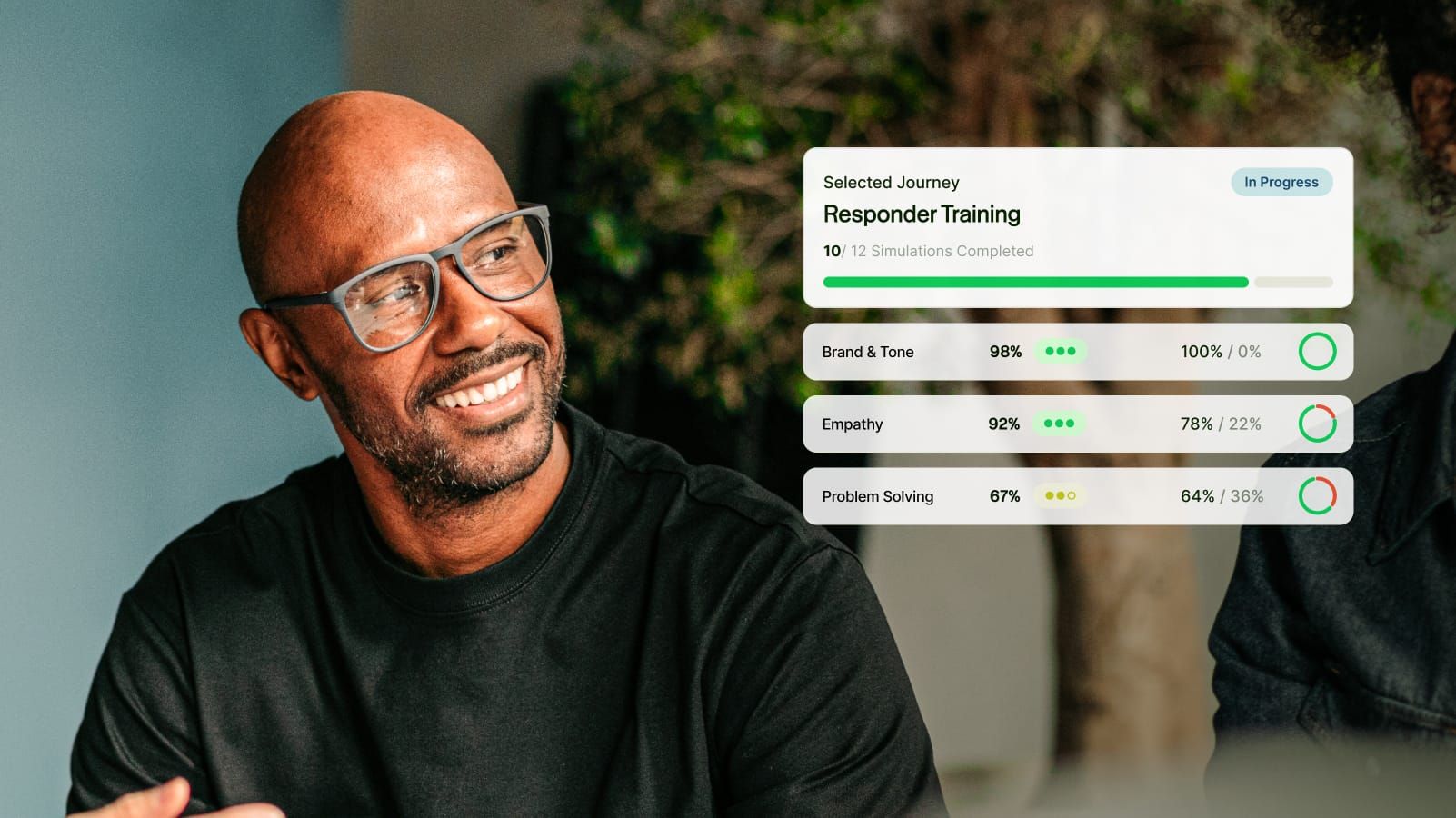
Specifically, ReflexAI simulations have helped to drive the following outcomes in healthcare settings and beyond.
- 90% improvement in team communication
- 80% increase in team confidence
- 59%+ faster onboarding
If you’re ready to explore how AI simulation-based training can transform your hospital system training programs, request a demo.